The calculation of perfusion analysis is based on measurements taken while the bolus travels through the blood system. The starting point is the arterial input function (AIF), measured at the artery before the contrast agent bolus travels through the region of interest (ROI). Perfusion analysis from first-pass contrast enhancement kinetics requires modeling tissue contrast exchange. To streamline the integrated analysis of perfusion parameters, there is a present a visual analysis approach incorporating pre-processing and statistical methods. Motion correction and noise reduction are fundamental pre-processing issues to achieve a reliable correspondence of voxels over time. Since the different parameters are derived from the same TIC (time-signal intensity curve), it is likely that some parameters correlate with each other.
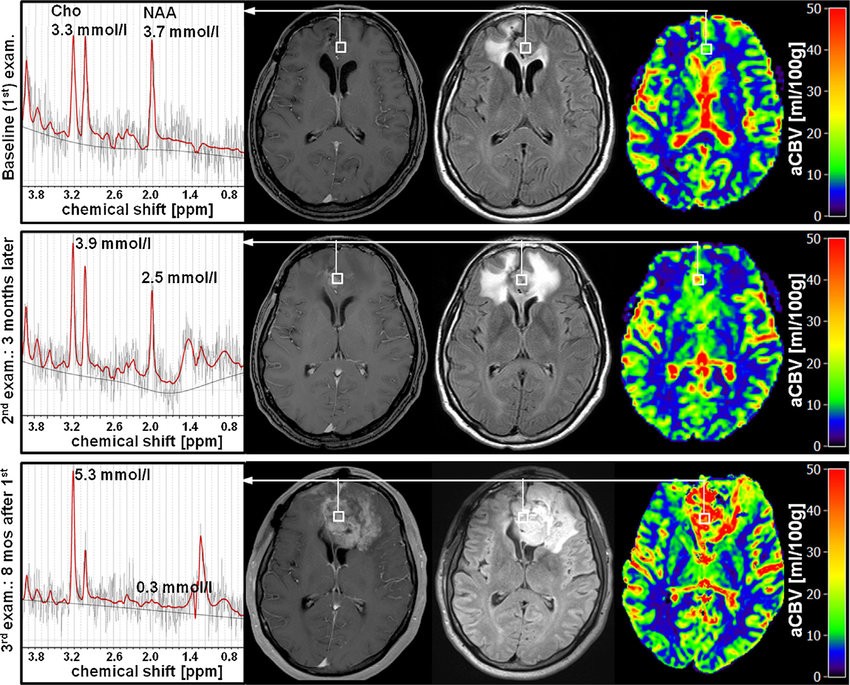
When interpreted in the context of DWI and conventional imaging, this visual TIC analysis can be quite useful in helping to distinguish such lesions from GBM and oligodendroglioma. In a rim-enhancing lesion, peripheral rCBV less than or equal to that of the surrounding WM should suggest the possibility of abscess and indicates a need for careful correlation with DWI, MRS, and anatomic images. The usefulness of rCBV to distinguish glioma from metastases remains undefined. Published data show that the rCBV of metastases varies with the vascularity of the primary tumor in a range overlapping that of GBM.
Another venue of analyzing perfusion data relates to a statistical analysis as well as mining and knowledge discovery techniques. The particular advantage of quantitative analysis in this context is the independence from the clinical information.
Perfusion-analysis software is widely available in clinical practice; however, it is often treated as a black box tool. Some of this software incorporates mathematical techniques to deal with contrast agent leakage. The values produced are generally accepted, but validation is challenging. The rCBV thresholds for differentiating progression vs pseudoprogression or tumor grading are often not the same across different perfusion-analysis software packages because different software packages utilize different methodologies for estimating bolus entrance and exit times, and determining baselines, model fitting, integration methods, and mathematical models to correct for contrast-agent extra-vasation. To acquire imaging data that can be used for a perfusion analysis, the requirements that are necessary for the scanner are generally not very specific. Some technical considerations must be fulfilled to allow raw data acquisition for the different methods. Perfusion analysis can help clinicians estimate treatment response and develop therapeutic pathways designed specifically for individual patients. For perfusion analysis to be effective and accurate, the data needs to be taken with an imaging modality capable of acquiring temporally uniform dynamic images of the entire anatomy, have sufficient temporal sampling.
There are several types of de-convolution that can be used for perfusion analysis. Singular Value Decomposition (SVD) algorithms are often viewed as the most accurate method because they do not rely on assumptions about the shape of the residue function. Some of the problems associated with standard SVD algorithms for brain perfusion are: noise sensitivity, inaccurate MTT values due to autoregulation or collateral flow, and inability to account for natural blood flow dynamics.
In the process of analysis of PCT maps, neuro-radiologists detect, measure, and describe the asymmetry between perfusion in left and right hemisphere of the patient. This process is currently done manually. In order to perform a perfusion image analysis, it is necessary to find the lines that separate the left brain hemisphere from the right one. Statistical evaluation with region of interest measurements is also possible with the digital phantom, and the accuracy of the perfusion analysis can be determined by calculating correlations with true values, as well as error sources. Variations in the absolute values may be partly caused by the difference in basic algorithms, such as SVD and maximum slope, as well as other minor implementations in perfusion analysis.
Standardization of perfusion analysis is important for multi-center trials. If different programs produce different perfusion results, perfusion images cannot be used for patient selection and final infarction. On the other hand, if standardization is achieved, the results obtained in one study with the use of one software package can be applied to another study with the use of a different program. A digital phantom is a useful tool for evaluating the accuracy and characteristics of CT perfusion and perfusion-weighted imaging perfusion analysis software. Phantom analysis reveal that all the commercial programs for CT perfusion and perfusion weighted imaging showed delay-induced errors.
Cerebral perfusion analysis is used in neuro-radiology to assess tissue level perfusion and delivery of blood to the brain and/or tissues of the head. A perfusion CT study involves sequential acquisition of CT sections during intravenous administration of an iodinated contrast agent. The procedure involves injecting a contrast agent into the individual. While investigators were instructed not to use the perfusion maps generated by the automated CT perfusion analysis software for decision-making regarding endovascular therapy, they could use their standard of care perfusion software for this purpose.
What is perfusion weighted imaging? Perfusion-weighted imaging (PWI) MRI is a noninvasive MR technique that allows measurement and examination of cerebral perfusion with assessment of various hemodynamic parameters, such as cerebral blood volume, cerebral blood flow, mean transit time, and time to peak.
What is brain perfusion CT scan? Computed tomography (CT) perfusion of the head uses special x-ray equipment to show which areas of the brain are adequately supplied with blood (perfused) and provides detailed information about blood flow to the brain. CT perfusion is fast, painless, noninvasive and accurate.
What does perfusion mean? 1. The circulation of blood through tissues. 2. Passing of a fluid through spaces. Supplying of an organ or tissue with nutrients and oxygen by injecting blood or a suitable fluid into an artery.